Capital Area Public Health Network
- 410 pages
- Not For Public Distribution
- July 2009
F. Mass Immunization, Prophylaxis and Pharmaceutical Dispensing
The Capital Area Public Health Network is planning for the immunization or prophylaxis of the entire population in the region. This plan will serve a guide for a regional response to a local or regional event in the Capital Area. The plan is flexible to adjust to the scope of the event. POD response time and target numbers are specific to the particular event. These variables will dictate how many POD sites will be activated. This plan prepares for the worst-case scenario by identifying five POD sites located throughout the region to be used in large-scale emergencies. In order to balance clinic load, reduce congestion, and maximize facility operations, residents have been assigned to a specific POD by municipality.
…
…
Annex F Isolation and Quarantine
3. Isolation
Isolation is defined as the physical separation and confinement of an individual, group of individuals, or individuals present within a geographic area who are infected with a communicable disease or are contaminated or whom the Commissioner of DHHS reasonably believes to be infected with a communicable disease or to be contaminated, in order to prevent or limit the transmission of the disease to the general public.
Types of Isolation include:
- Home Isolation
- Isolation in a community facility
- Hospital Isolation
3.1 Home Isolation
It may be preferable for affected individuals to be monitored in their own homes, if certain requirements are met. For example, if there is an immunosuppressed person also inhabiting the home, monitoring in an alternate, non-hospital facility may be necessary. An example of a feasible alternate lodging facility may include a motel room, with a separate entrance to the outside/outdoors, a private bathroom, perhaps a small refrigerator and/or microwave, and communication capabilities to the outside (by telephone).
Before a case is confined to the home, the residence should be assessed to be certain that it has the features necessary for the provision of proper care and proper infection control measures. The primary caregiver, the case himself or herself, or a public health worker may conduct this assessment.
Isolation facilities should meet the following minimum requirements:
o Primary caregiver (family member) available, if necessary, to assist the patient with basic needs.
o Functioning telephone, electricity, and drinkable water.
o Separate bedroom that will be occupied only by the case and with a door that can be kept closed at all times.
o Separate bathroom that is designated for use only by the case.During the period of isolation, household members of cases who are not providing care to the patient-case should be relocated, if possible. Alternatively, the case patient could be relocated to another site within the region (a motel room). If relocation is not possible, then interactions between the case and the household members should be minimized. Persons at risk of serious complications should not interact with the case patient. All persons in contact with the case should be educated regarding appropriate infection control practices, including hand hygiene, Personal Protective Equipment (PPE) and environmental
decontamination.3.2 Isolation in a Community Facility
If the isolation capacity is exceeded at the hospitals, an Acute Care Center could be established to provide supportive care to patients that would not be able to stay at home, but would not need the level of care provided at an acute care hospital.
Primary Site: Edna McKenna Jail – Merrimack County
Daniel Webster Highway, Boscawen
See Annex E for Acute Care Center Plan3.3 Hospital Capacity & Isolation
Current Isolation Capacity:
Concord Hospital has 22 rooms that have the capability of creating a negative pressure environment. It also the capacity to create an additional 13 negative pressure beds through the use of portable isolation units. NH Hospital has the capacity to isolate 20 individuals in a negative pressure environment but is only able to provide supportive care.
Cohorting patients may be difficult to accomplish in many hospitals, and each hospital will develop its own plan based on resources (personnel, facility design, etc.). The following is CDC’s suggested hierarchical approach:
- When possible, place patients with documented or suspected disease in a private room.
- When the number of patients with disease exceeds the available private rooms, try to place cases together in multi-bed rooms or wards.
- When patients with and without disease must be placed in a room together, try to avoid including uninfected patients most susceptible to complications.
- When multiple cases are admitted, minimize the number of staff having contact with infected patients by assigning all case patients to a single or small group of health care personnel, who have been given prophylaxis (if medications available and appropriate).
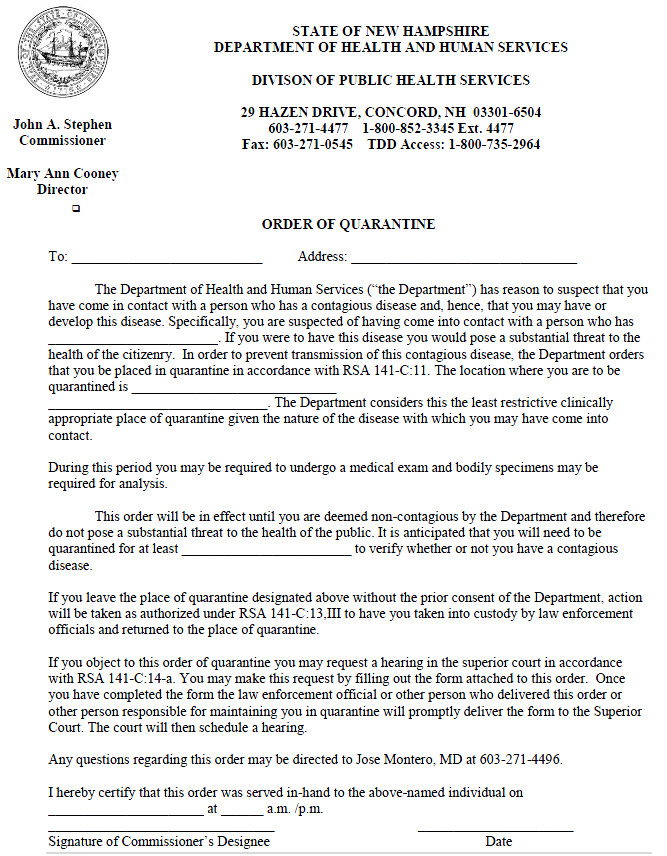
4. Quarantine
Quarantine is defined as the physical separation and confinement of an individual, group of individuals, or individuals present within a geographic area who are exposed to a communicable disease or are contaminated, or whom the commissioner of DHHS reasonably believes have been exposed to a communicable disease or to be contaminated or have been exposed to others who have been exposed to a communicable disease or contamination, to prevent transmission of the disease to the general public. The decision of whether or not to quarantine or isolate individuals will be based primarily on the type of event and the nature of the disease agent.
Quarantine represents a range of possible interventions that could be applied at the level of the individual, small group, or community. Quarantine may be used for:
- Individuals with close contact (e.g., household contact) to a known case.
- Small groups with close contact (e.g., co-workers, health care workers with unprotected exposure) to a case.
- Larger groups with an unspecified extent of exposures (e.g., social groups, persons in congregate settings, passengers on airplanes) to a case.
- Communities in which the extent of exposure for individuals is unknown but interventions are needed to control potential population exposures by increasing social distance and limiting interactions and movement within a community.
- Local law enforcement enforces State issued quarantine/isolation orders (RSA 141-C:13, III).
Types of quarantine include:
- Home Quarantine
- Quarantine in Community Facilities
- Work Quarantine
4.1 Home quarantine
Quarantine at home is most suitable for contacts that have a home environment in which their basic needs can be met and where the protection of unexposed household members is feasible. The minimum criteria that must be met to enable the optimal implementation of home quarantine include:
- Access to educational materials about the disease in question
- Ability to monitor one’s own symptoms (or have them monitored regularly by a parent, guardian or caregiver)
- Basic utilities (water, electricity, functional plumbing/septic system, garbage collection, and heating and air conditioning as appropriate)
- Basic supplies (clothing, food, hand hygiene supplies, laundry services, etc.)
- Mechanisms for communication, including telephone (for monitoring by health staff, reporting of symptoms, and accessing support services) and a computer if possible
- Access to food and food preparation
- Access to health care providers, health care centers, and ambulance personnel
- Access to supplies such as thermometers, fever logs, phone numbers for reporting symptoms or accessing services, emergency numbers, etc.
- Availability of mental health/psychological support services
No specific precautions are needed for household members of contacts who are in home quarantine, as long as the person under quarantine remains asymptomatic. Household members of quarantined individuals can go to school, work, etc., without restrictions. If the contact develops symptoms, then s/he should immediately notify medical/public health authorities to obtain medical evaluation, and at that point, household members should remain at home.
4.2 Quarantine in Community Facilities
Contacts who do not have an appropriate home environment for quarantine or contacts who do not wish to be quarantined at home may be quarantined in specific facilities (motels, nursing homes, apartments, etc.) designated for this purpose. A location has been identified that could provide food and shelter for 00 individuals requiring quarantine but don’t have the resources to stay at home.
Primary Site: Philbrook Center (NH Hospital Campus)
36 Clinton St Concord NH
Tel: 271-5300See Appendix 4 for Quarantine Center Plan
4.3 Work Quarantine
This applies to health care workers or other essential personnel who have been exposed to cases and who may need to continue working (with appropriate infection control precautions) but who are quarantined either at home or in a designated facility during off-duty hours.
…
ANNEX G Mass Casualty Management
Purpose: Develop a plan for the Capital Area to address a public health emergency that results in mass fatalities that overwhelm the current system
Issues:1. Storing Remains
- Identification of temporary refrigerated storage facilities
- The State of NH Mass fatality workgroup will be identifying vendors to supply refrigerated trucks
- Racks to be built to fit into trucks. Each truck could hold 24 bodies.
- Placement of refrigerator trucks
- The region will be able to house five refrigerator trucks to be located at Local Fire or Police Departments
- Suggested locations: Hillsboro, Loudon, Pembroke, Pittsfield, Webster (using POD regions to determine towns)
- Securing trucks
- Local Police will handle security of trucks
- Neighboring towns will contact hosting town when a delivery is to be made
- Tracking remains
- Bar code system, waterproof tags, etc.
2. Assessing current capacity of region
- Funeral homes
- Storage/morgue capacity
- Transportation capacity (# vehicles/drivers)
- Crematory capacity
- Embalming capacity
- Body bag inventory (heavy duty/regular)
- Transportation providers
- Ability to transport remains
1. EMS
2. Other healthcare agencies
- Notification
- County Attorne
- Medical Examiner
3. Handling Remains
- Personal Protective Equipment
- Personal Effects
- Transportation
4. Processing Remains
- Family Support/Assistance
- Look into using Neighborhood Emergency Help Center
- Maintain honor, dignity with an awareness of religious belief systems
- Burial (embalming) vs. cremation
- Standard burials vs. mass burials
- Standard services vs. delayed services
- Maintain processing the daily case load
5. Communication
- Maintain communication pathways between
- County Attorney
- Medical Examiner
- Hospital
- Physicians
- Funeral Directors
- Police
- EMS